Join Us Live for a Discussion on Medicare, Democracy, and the Future of Health Care
Leveling the Playing Field With Site Neutral Medicare Payments

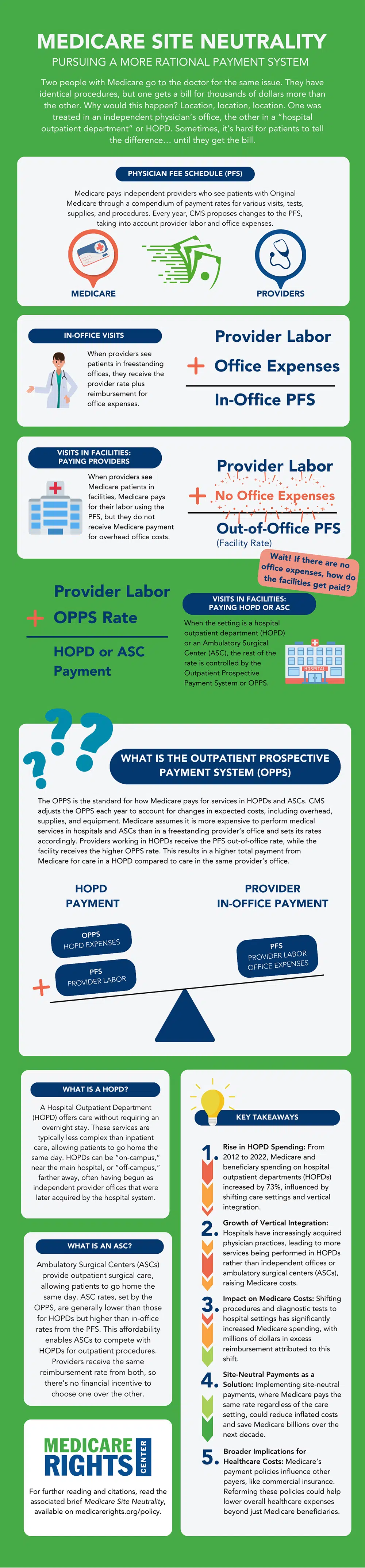
When Medicare pays for health services, there is one key factor that can cause a difference of thousands of dollars for procedures that are otherwise identical: location. Where a person receives care and how that provider is classified under Medicare’s payment structure is that hidden key. Medicare typically pays hospital outpatient departments (HOPDs) more than independent physicians’ offices, even when the services provided are the same. This creates incentives for hospitals to buy up physician practices or use other strategies to funnel patients to more profitable sites. Over time, this drives up taxpayer and beneficiary spending, resulting in financial strain on the Medicare program.
Part 3: Medicare Site Neutrality
The third and final part of the Medicare Rights Center’s policy series on Medicare sustainability examines the financial consequences of current site-specific payment rules and advocates for a more rational payment system. Comparing the rates of reimbursement for three categories of provider locations—independent physicians’ offices, ambulatory surgical centers (ASCs), and HOPDs—the Part 3 issue brief outlines policy directions for more sustainable payment systems across outpatient Medicare services.
Unequal Payment Between Settings
The Physician Fee Schedule (PFS) determines the rates at which Original Medicare reimburses clinicians, both for their labor and for overhead office expenses. When independent physicians see patients in freestanding offices, they receive the PFS “in-office” rate. However, when the same care is delivered in an ASC or HOPD, both of which are considered “facilities” under Medicare’s payment structure, a second set of reimbursement rules comes into play: the Outpatient Prospective Payment System.
Practitioners who work in these facilities receive the “out-of-office” PFS rate—the portion of the PFS that accounts for the cost of their labor—and the facility receives the OPPS rate for office expenses. This rate is much higher than the corresponding office reimbursement offered by the PFS, paying ASCs more than freestanding offices and HOPDs even more than ASCs. This can cause the total bill for a visit to be two or three times higher than that for the same service provided by a clinician in a freestanding office.
This narrowing of the provider field increases costs for Medicare, taxpayers, and beneficiaries.
This means that hospitals have been incentivized to buy up formerly independent physicians’ practices and vertically integrate them, referring patients within their hospital systems and, in turn, driving down traffic to remaining independent practices and ASCs. The numbers bear this out; HOPD services have expanded dramatically and take up an increasing share of Medicare outpatient spending. From 2012 to 2022, spending on hospital outpatient services increased by 73%, and as of 2022, hospitals owned 53.6% of physician practices, a sharp increase from 38.8% in 2019. This narrowing of the provider field increases costs for Medicare, taxpayers, and beneficiaries—and benefits only the hospital systems pursuing the higher site-specific payments.
Sustainability Reforms Require Changing Initiatives
As described in the first part of our Medicare Sustainability policy series, Part B outpatient services now account for the greatest share of Medicare spending, and the demands on Part B spending are only growing. Site neutrality is a crucial policy reform that will create savings in Part B spending—the Government Accountability Office estimates such changes could save $141 billion over 10 years—by ensuring that identical outpatient procedures across independent offices and hospital departments are reimbursed at the same rate. Ultimately, these solutions seek to improve payment accuracy and reduce overpayment by removing the financial incentive for hospitals to vertically integrate and absorb routine care services that could have been provided at a lower cost.
Ensuring Medicare’s sustainability requires policy-driven changes that shift the incentive structures for insurance companies and facilities.
Similarly, the policy reforms outlined in the second part of our series, against Medicare Advantage (MA) proliferation, also seek to systemically reduce the incentives driving insurers to flood the market with MA plans and profit from overpayments. Limiting plan proliferation through regulations and strengthening public, federally funded sources of counseling and information will enable people to make better coverage choices and avoid reliance on biased information.
Ensuring Medicare’s sustainability requires policy-driven changes that shift the incentive structures for insurance companies and facilities. As long as the rules continue to allow overpayments and arbitrary cost inflation, Medicare and those it serves will continue to shoulder an increasing burden.
For more on site neutrality, view Part 3 of the Medicare Sustainability policy series available at https://www.medicarerights.org/policy-series/medicare-sustainability.
Explore the Infographic
Show Comments
We welcome thoughtful, respectful discussion on our website. To maintain a safe and constructive environment, comments that include profanity or violent, threatening language will be hidden. We may ban commentors who repeatedly cross these guidelines.
Help Us Protect & Strengthen Medicare
Donate today and make a lasting impact
More than 67 million people rely on Medicare—but many still face barriers to the care they need. With your support, we provide free, unbiased help to people navigating Medicare and work across the country with federal and state advocates to protect Medicare’s future and address the needs of those it serves.
The Latest
Most Read
Add Medicare to Your Inbox
Sign up to receive Medicare news, policy developments, and other useful updates from the Medicare Rights.
View this profile on InstagramMedicare Rights Center (@medicarerights) • Instagram photos and videos









