March 16 National Call-In Day: Tell Congress to Protect Our Care
Congressional leaders are rushing to enact a plan that would rip health coverage away from 24 million Americans, impose an
Join Us Live for a Discussion on Medicare, Democracy, and the Future of Health Care
Medicare Watch articles are featured in Medicare Rights’ weekly newsletter, which helps readers stay updated on Medicare policy and advocacy developments and learn about changes in Medicare benefits and rules. Subscribe now by visiting www.medicarerights.org/newsletters.
Congressional leaders are rushing to enact a plan that would rip health coverage away from 24 million Americans, impose an

Earlier this week, the Congressional Budget Office (CBO) released its highly anticipated analysis of the American Health Care Act (AHCA) and what its passage would mean for American families. The CBO estimate confirms our worst fears—24 million people would lose health coverage over the next decade.
The report affirms that older adults will be among those hardest hit by the proposal. If the AHCA becomes law, the number of uninsured would increase most significantly among low-income Americans ages 50 to 64.

This week, two prominent policy organizations published articles on how the American Health Care Act (AHCA)—the Republican bill put forward to repeal the Affordable Care Act (ACA)—would change the Medicare program. The Kaiser Family Foundation (KFF) and the Center on Budget and Policy Priorities (CBPP) identify the AHCA’s Medicare provisions and illustrate the potential impact of the changes.

Earlier this week, Congressional Republicans unveiled their plan to repeal the Affordable Care Act (ACA), known as the American Health Care Act (AHCA). Only two day later, the bill was debated and voted on by the House Committees on Energy & Commerce and Ways & Means. In response, Joe Baker, president of the Medicare Rights Center (Medicare Rights), sent a letter to the Committee leadership explaining why Medicare Rights cannot support the legislation or the process behind it.

The Centers for Medicare & Medicaid Services (CMS) recently announced a time-limited opportunity allowing Medicare-eligible people who were or are currently enrolled in the Affordable Care Act’s Marketplaces to enroll in Medicare Part B and to be relieved of any associated late enrollment penalties.
This chance to request equitable relief is welcome news for Marketplace enrollees who wrongly delayed or declined Medicare Part B enrollment. The relief may include retroactive or immediate Medicare Part B enrollment and a reduction in or elimination of Medicare Part B late enrollment penalties. People who were or are enrolled in Marketplace coverage and who are entitled to premium-free Medicare Part A can apply for this relief through September 2017.
This week, the Medicare Rights Center (Medicare Rights) submitted comments in response to the Centers for Medicare & Medicaid Services (CMS) 2018 Advance Rate Notice and Draft Call Letter (2018 Call Letter). CMS announces proposed changes to the Medicare Advantage (MA) and Part D programs through a yearly call letter, and every year Medicare Rights provides feedback to the agency on proposals we support and where we have concerns.

Last week, the Kaiser Family Foundation (KFF) released an issue brief on the effects Medicaid expansion under the Affordable Care Act (ACA) had on coverage, access to care, and economic outcomes. In the brief, KFF reviews the findings of over 100 studies of the impact of states extending the eligibility of the Medicaid program to low-income adults between ages 19 and 64.
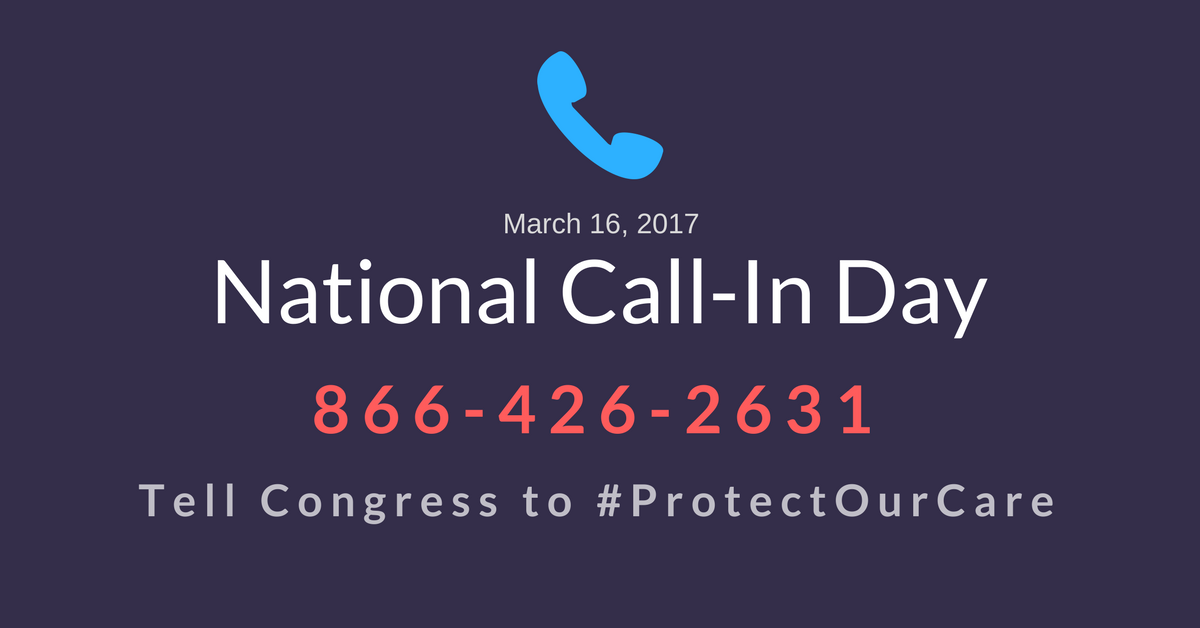
Today, the Medicare Rights Center released its annual helpline trends report, which outlines persistent challenges facing people with Medicare heard through thousands of calls to its national consumer helpline.
The report, Medicare Trends and Recommendations: An Analysis of 2015 Call Data from the Medicare Rights Center’s National Helpline, highlights the leading issues heard on Medicare Rights’ helpline. Each issue is demonstrated through consumer stories and accompanied by policy solutions, which the Centers for Medicare & Medicaid Services (CMS), state agencies, insurers, elected officials, and others can pursue to improve the Medicare program for the more than 55 million people it serves.

Currently, people with Medicare are all entitled to the same set of basic benefits, and the program treats all people with Medicare equally. Some policymakers support changing Medicare into a premium support program, which would mean people with Medicare would receive a voucher to purchase health coverage through a private plan or Original Medicare.
As policymakers continue to debate the future of our country’s health care system, some policymakers endorse proposals to give Medicare providers the right to charge seniors and people with disabilities more for their care through balance billing or private contracting. Under these plans, Medicare providers could require patients to negotiate a contract for the cost of their care, and people with Medicare would have additional payments on top of their premiums, copayments, and coinsurance. Unless they successfully negotiate otherwise, patients would also be responsible for filing the Medicare claim.
Congressional leaders are rushing to enact a plan that would rip health coverage away from 24 million Americans, impose an

Earlier this week, the Congressional Budget Office (CBO) released its highly anticipated analysis of the American Health Care Act (AHCA) and what its passage would mean for American families. The CBO estimate confirms our worst fears—24 million people would lose health coverage over the next decade.
The report affirms that older adults will be among those hardest hit by the proposal. If the AHCA becomes law, the number of uninsured would increase most significantly among low-income Americans ages 50 to 64.

This week, two prominent policy organizations published articles on how the American Health Care Act (AHCA)—the Republican bill put forward to repeal the Affordable Care Act (ACA)—would change the Medicare program. The Kaiser Family Foundation (KFF) and the Center on Budget and Policy Priorities (CBPP) identify the AHCA’s Medicare provisions and illustrate the potential impact of the changes.

Earlier this week, Congressional Republicans unveiled their plan to repeal the Affordable Care Act (ACA), known as the American Health Care Act (AHCA). Only two day later, the bill was debated and voted on by the House Committees on Energy & Commerce and Ways & Means. In response, Joe Baker, president of the Medicare Rights Center (Medicare Rights), sent a letter to the Committee leadership explaining why Medicare Rights cannot support the legislation or the process behind it.

The Centers for Medicare & Medicaid Services (CMS) recently announced a time-limited opportunity allowing Medicare-eligible people who were or are currently enrolled in the Affordable Care Act’s Marketplaces to enroll in Medicare Part B and to be relieved of any associated late enrollment penalties.
This chance to request equitable relief is welcome news for Marketplace enrollees who wrongly delayed or declined Medicare Part B enrollment. The relief may include retroactive or immediate Medicare Part B enrollment and a reduction in or elimination of Medicare Part B late enrollment penalties. People who were or are enrolled in Marketplace coverage and who are entitled to premium-free Medicare Part A can apply for this relief through September 2017.
This week, the Medicare Rights Center (Medicare Rights) submitted comments in response to the Centers for Medicare & Medicaid Services (CMS) 2018 Advance Rate Notice and Draft Call Letter (2018 Call Letter). CMS announces proposed changes to the Medicare Advantage (MA) and Part D programs through a yearly call letter, and every year Medicare Rights provides feedback to the agency on proposals we support and where we have concerns.

Last week, the Kaiser Family Foundation (KFF) released an issue brief on the effects Medicaid expansion under the Affordable Care Act (ACA) had on coverage, access to care, and economic outcomes. In the brief, KFF reviews the findings of over 100 studies of the impact of states extending the eligibility of the Medicaid program to low-income adults between ages 19 and 64.
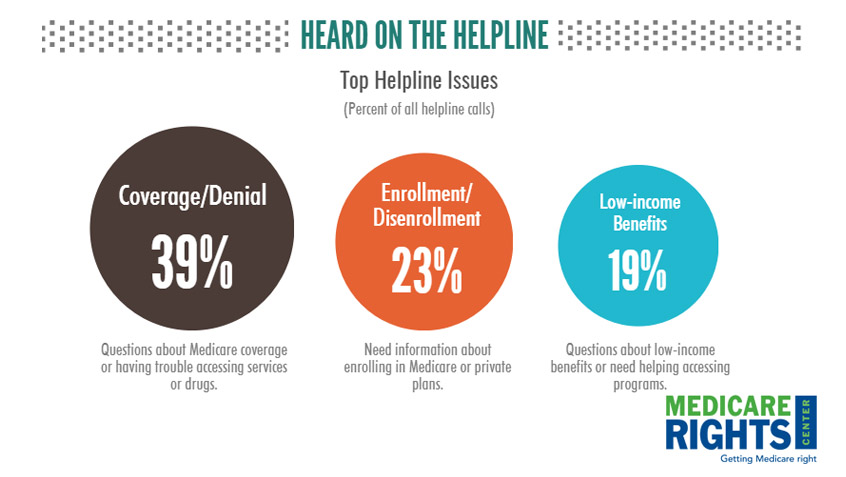
Today, the Medicare Rights Center released its annual helpline trends report, which outlines persistent challenges facing people with Medicare heard through thousands of calls to its national consumer helpline.
The report, Medicare Trends and Recommendations: An Analysis of 2015 Call Data from the Medicare Rights Center’s National Helpline, highlights the leading issues heard on Medicare Rights’ helpline. Each issue is demonstrated through consumer stories and accompanied by policy solutions, which the Centers for Medicare & Medicaid Services (CMS), state agencies, insurers, elected officials, and others can pursue to improve the Medicare program for the more than 55 million people it serves.

Currently, people with Medicare are all entitled to the same set of basic benefits, and the program treats all people with Medicare equally. Some policymakers support changing Medicare into a premium support program, which would mean people with Medicare would receive a voucher to purchase health coverage through a private plan or Original Medicare.
As policymakers continue to debate the future of our country’s health care system, some policymakers endorse proposals to give Medicare providers the right to charge seniors and people with disabilities more for their care through balance billing or private contracting. Under these plans, Medicare providers could require patients to negotiate a contract for the cost of their care, and people with Medicare would have additional payments on top of their premiums, copayments, and coinsurance. Unless they successfully negotiate otherwise, patients would also be responsible for filing the Medicare claim.