Join Us Live for a Discussion on Medicare, Democracy, and the Future of Health Care
CMS Announces New Rules That Could Make Part D Drug Formularies Much More Complicated
This week, the Centers for Medicare and Medicaid Services (CMS) announced that, starting in 2020, Part D Plans and Medicare Advantage Plans with Part D will be able to include medications on their formulary for some FDA-approved uses, but not others. Currently, a plan can favor one drug over another by including a medication on its formulary or not; placing it on a lower cost sharing tier; or putting coverage restrictions, like prior authorization, quantity limits, or step therapy on the less preferred medication. These rules apply uniformly to each drug, for all FDA- and compendia-approved purposes—the new rules do not.
For example if drug A is FDA approved for two uses—one to treat condition X and one to treat condition Y—plans must include drug A on the formulary for X and Y or exclude it for both X and Y. Under the new rules, however, plans will be able to treat a prescription for a drug to treat X differently from the same prescription to treat Y.
CMS indicates that their intent is to increase a plan’s ability to negotiate indication-specific drug prices, but there are few details about how these differences will be communicated to beneficiaries. The memo from CMS states that if plans wish to use this type of formulary design they must “disclose that some drugs may be subject to those requirements in the plan’s Annual Notice of Change (ANOC) and Evidence of Coverage (EOC) documents.”
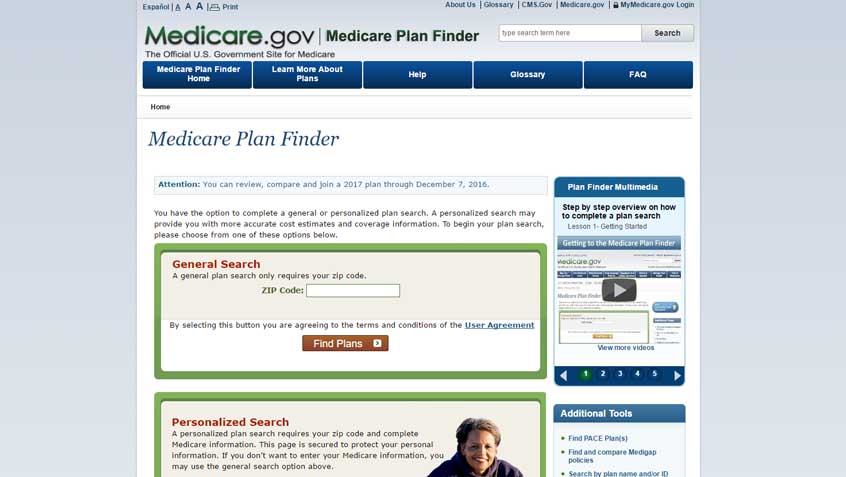
We believe this is inadequate – CMS should require integration of this information, including asking about the conditions for which drugs are prescribed, in the Medicare Plan Finder tool. Plans should also be required to designate any drugs that have indication-based restrictions in their online and print formularies.
Medicare Rights is concerned that people with Medicare will face ever-growing difficulties in choosing what coverage is right for them. Already, many people struggle with their coverage decisions, and new complex plan offerings are likely to increase these problems.
Show Comments
We welcome thoughtful, respectful discussion on our website. To maintain a safe and constructive environment, comments that include profanity or violent, threatening language will be hidden. We may ban commentors who repeatedly cross these guidelines.
Help Us Protect & Strengthen Medicare
Donate today and make a lasting impact
More than 67 million people rely on Medicare—but many still face barriers to the care they need. With your support, we provide free, unbiased help to people navigating Medicare and work across the country with federal and state advocates to protect Medicare’s future and address the needs of those it serves.
The Latest
Most Read
Add Medicare to Your Inbox
Sign up to receive Medicare news, policy developments, and other useful updates from the Medicare Rights.
View this profile on InstagramMedicare Rights Center (@medicarerights) • Instagram photos and videos









