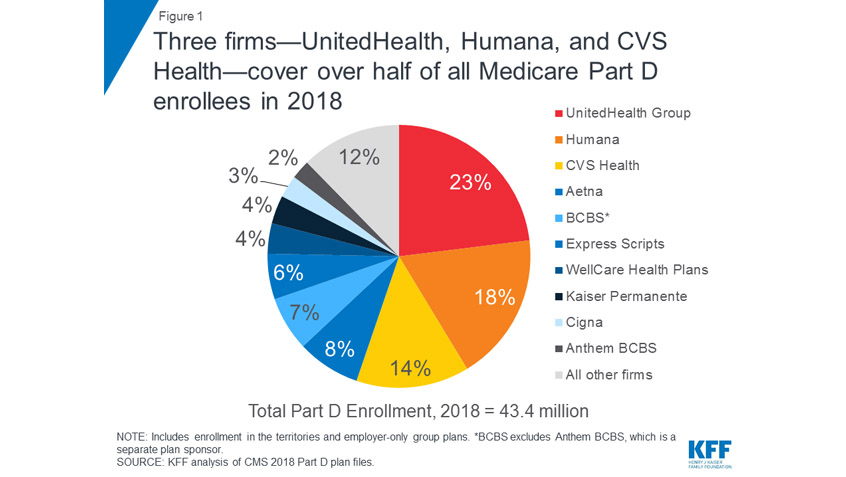
This week, Avalere Health, a Washington DC-based consulting firm that specializes in strategy, policy, and data analysis, released a study on the impact of moving the coverage of some drugs from Medicare Part B to Part D. While most drugs are covered under the Part D prescription drug program, Part B, the part of the Medicare program that covers outpatient medical services like office visits, covers a few. The drugs covered by Part B are usually ones that beneficiaries would not give to themselves. For example, if a provider administers the drug during an office visit, Part B instead of Part D, might cover that drug.
Earlier this month, the Trump Administration announced it would consider transitioning certain Part B drugs into Part D as part of a larger strategy to lower drug prices and out-of-pocket costs. This makes it essential to understand what effects the switch could have on people with Medicare.