
OIG Releases Troubling Reports on Medicare Hospice Benefit
The Department of Health and Human Services, Office of Inspector General (OIG) recently released two reports on the Medicare hospice
Join Us Live for a Discussion on Medicare, Democracy, and the Future of Health Care



The Department of Health and Human Services, Office of Inspector General (OIG) recently released two reports on the Medicare hospice

This week, the U.S. Court of Appeals for the Fifth Circuit heard oral arguments in Texas v. U.S., the latest legal challenge

This week, the House Committee on Ways and Means advanced the Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act (S. 1280/H.R. 2477) in a markup that considered a series of Medicare-related bills. The BENES Act is now included in a larger bipartisan package that was unanimously reported favorably out of Committee—the Beneficiary Education Tools, Telehealth, and Extenders Reauthorization (BETTER) Act of 2019 (H.R. 3417).

This week, the Center for Medicare Advocacy released a new resource on the Medicare Improvement Standard. The issue brief, “Implementing Jimmo v. Sebelius: An Overview Settlement implementation,” is intended to provide Medicare stakeholders with an overview of the Jimmo Settlement, what it means in different care settings, and links and references to helpful resource materials.

The Medicare Rights Center applauds Senators Ben Cardin (D-MD) and John Cornyn (R-TX) for introducing the bipartisan Streamlining Part D Appeals Process Act (S. 1861).
The bill would eliminate unnecessary steps in the Medicare Part D appeals process, making the system less burdensome for people with Medicare, providers, and plans. Specifically, the Cardin-Cornyn bill would simplify the process for Part D enrollees who experience medication denials at the pharmacy counter.
In its June 2019 report to Congress, the Medicare Payment Advisory Commission (MedPAC) recommends improvements to the complex Medicare Part B enrollment process, including strengthening notification requirements which is, in part, what the Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act proposes to do (S. 1280/H.R. 2477).

Earlier this year, a federal government systems issue prevented Medicare Advantage and Part D premiums from being automatically deducted from the Social Security payments of some people with Medicare. Normally, if a beneficiary elects, Social Security deducts the premiums and sends them directly to the plan. In this instance, the payments were not sent to the plans, and beneficiaries did not know that their plans were not receiving them.
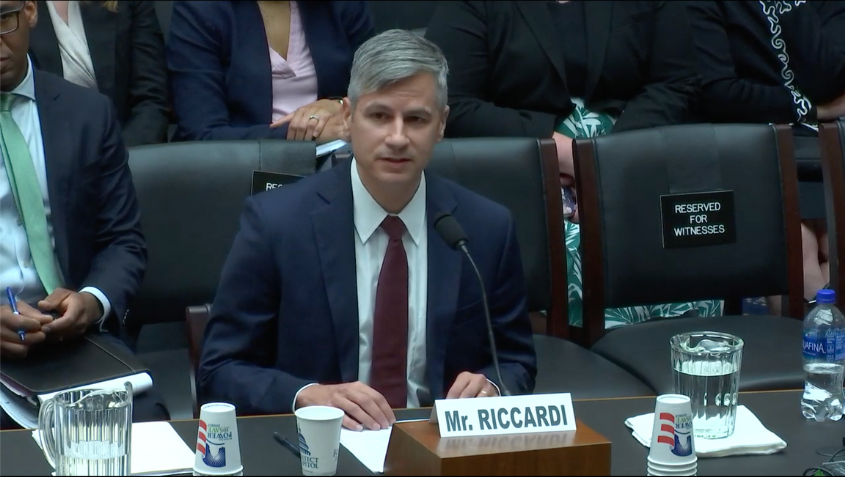
On June 4, Medicare Rights Center President Fred Riccardi testified at a hearing of the House Committee on Energy and Commerce, Subcommittee on Health titled “Investing in America’s Health Care.”
The hearing examined an array of public health initiatives set to expire in September. Riccardi spoke to several of the Medicare-related programs, urging Congress to address these expirations in a health care “extenders” legislative package later this year.

A new issue brief from the Kaiser Family Foundation indicates that people with Medicare who choose Medicare Advantage (MA) plans have lower Medicare spending and use fewer services relative to their peers with Original Medicare, even before they enroll in MA.

The Medicare Trustee’s report underscores what we already know: Medicare is strong and built to last. We urge lawmakers to pursue commonsense reforms—like reversing the tax bill’s troubling trajectory, reigning in high prescription drug prices, and eliminating Medicare Advantage overpayments—to ensure it stays that way.

The Department of Health and Human Services, Office of Inspector General (OIG) recently released two reports on the Medicare hospice

This week, the U.S. Court of Appeals for the Fifth Circuit heard oral arguments in Texas v. U.S., the latest legal challenge

This week, the House Committee on Ways and Means advanced the Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act (S. 1280/H.R. 2477) in a markup that considered a series of Medicare-related bills. The BENES Act is now included in a larger bipartisan package that was unanimously reported favorably out of Committee—the Beneficiary Education Tools, Telehealth, and Extenders Reauthorization (BETTER) Act of 2019 (H.R. 3417).

This week, the Center for Medicare Advocacy released a new resource on the Medicare Improvement Standard. The issue brief, “Implementing Jimmo v. Sebelius: An Overview Settlement implementation,” is intended to provide Medicare stakeholders with an overview of the Jimmo Settlement, what it means in different care settings, and links and references to helpful resource materials.

The Medicare Rights Center applauds Senators Ben Cardin (D-MD) and John Cornyn (R-TX) for introducing the bipartisan Streamlining Part D Appeals Process Act (S. 1861).
The bill would eliminate unnecessary steps in the Medicare Part D appeals process, making the system less burdensome for people with Medicare, providers, and plans. Specifically, the Cardin-Cornyn bill would simplify the process for Part D enrollees who experience medication denials at the pharmacy counter.
In its June 2019 report to Congress, the Medicare Payment Advisory Commission (MedPAC) recommends improvements to the complex Medicare Part B enrollment process, including strengthening notification requirements which is, in part, what the Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act proposes to do (S. 1280/H.R. 2477).

Earlier this year, a federal government systems issue prevented Medicare Advantage and Part D premiums from being automatically deducted from the Social Security payments of some people with Medicare. Normally, if a beneficiary elects, Social Security deducts the premiums and sends them directly to the plan. In this instance, the payments were not sent to the plans, and beneficiaries did not know that their plans were not receiving them.
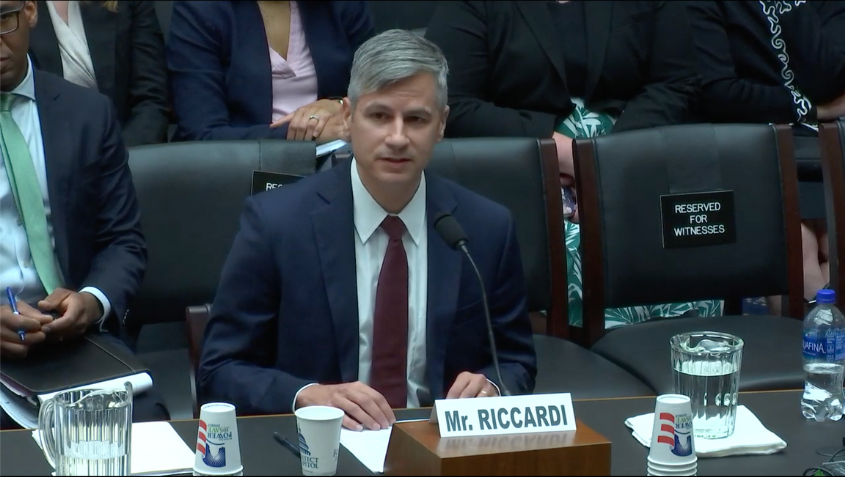
On June 4, Medicare Rights Center President Fred Riccardi testified at a hearing of the House Committee on Energy and Commerce, Subcommittee on Health titled “Investing in America’s Health Care.”
The hearing examined an array of public health initiatives set to expire in September. Riccardi spoke to several of the Medicare-related programs, urging Congress to address these expirations in a health care “extenders” legislative package later this year.

A new issue brief from the Kaiser Family Foundation indicates that people with Medicare who choose Medicare Advantage (MA) plans have lower Medicare spending and use fewer services relative to their peers with Original Medicare, even before they enroll in MA.

The Medicare Trustee’s report underscores what we already know: Medicare is strong and built to last. We urge lawmakers to pursue commonsense reforms—like reversing the tax bill’s troubling trajectory, reigning in high prescription drug prices, and eliminating Medicare Advantage overpayments—to ensure it stays that way.