Working in Washington to Improve Medicare
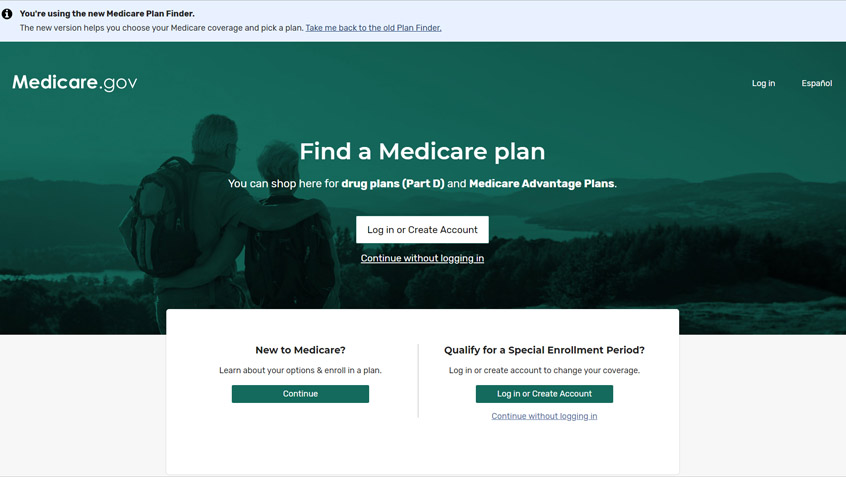
In recent months, the Medicare Rights Center has been pursuing urgently needed reforms, seeking to improve the federal coronavirus response and advance the bipartisan Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act (H.R. 2477/S. 1280).